A test for Lyme Disease | |||
 1,397 1,397  0 0  0 0 | |||
Two-Tiered Serological TestingThe most common approach to testing for Lyme disease involves a two-tiered serological process using blood tests. This method looks for antibodies your body produces in response to Borrelia burgdorferi, the bacterium responsible for Lyme disease.
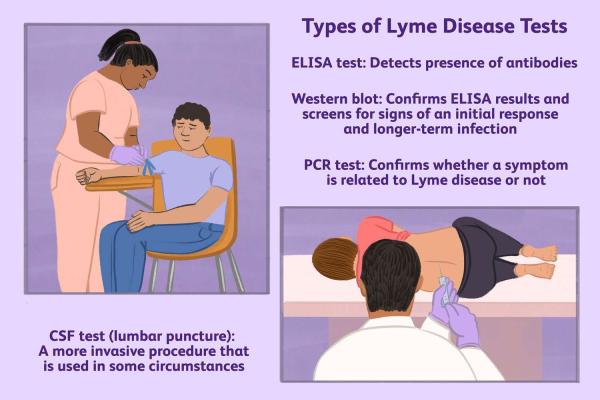
Enzyme-Linked Immunosorbent Assay (ELISA) or Immunofluorescence Assay (IFA)The first tier is an initial screening test, either an Enzyme-Linked Immunosorbent Assay (ELISA) or an Immunofluorescence Assay (IFA). A positive result on this test doesn't automatically confirm Lyme disease; it simply indicates the presence of antibodies to Borrelia burgdorferi. A negative result often suggests that Lyme disease is unlikely.
Western BlotIf the ELISA or IFA result is positive or borderline, a Western blot is performed as a confirmatory second-tier test. This test is more specific, looking for specific antibodies that strongly indicate Lyme disease. The interpretation of Western blot results requires expertise, as patterns of antibody bands are analyzed.
PCR (Polymerase Chain Reaction)PCR testing detects the actual DNA of Borrelia burgdorferi in a sample, such as blood, skin biopsy, or cerebrospinal fluid (CSF). While PCR can be useful, especially for testing CSF in suspected cases of neuroborreliosis (Lyme disease affecting the nervous system), it's not always reliable, particularly in later stages of infection. This is because the bacteria may not be consistently present in detectable amounts in the blood or other tissues.
Clinical EvaluationA thorough clinical evaluation is critical for accurate Lyme disease diagnosis. This involves the doctor considering the patient's symptoms, risk factors (such as exposure to ticks in Lyme-endemic areas), and physical findings. The characteristic "bulls-eye" rash (erythema migrans) is a strong indicator of Lyme disease, but it doesn't always appear. Therefore, its absence doesn't rule out the possibility of infection.
Important ConsiderationsSeveral factors can influence the accuracy and interpretation of Lyme disease tests:
False Positives and NegativesAll tests have limitations, including the possibility of false positive and false negative results. False positives can occur, especially in individuals with certain other conditions, such as autoimmune diseases. False negatives are more likely in the early stages of infection before the body has produced a sufficient antibody response, or if the test is performed too soon after exposure.
Stage of InfectionThe effectiveness of antibody testing can vary depending on the stage of infection. Early in the disease, antibody levels may be too low to be detected. PCR testing may be more useful in this stage.
Testing GuidelinesThe Centers for Disease Control and Prevention (CDC) and other health organizations provide specific guidelines for Lyme disease testing. Healthcare providers should adhere to these guidelines to ensure accurate and reliable results.
The Importance of Integrated DiagnosisDiagnosing Lyme disease requires a careful integration of test results with clinical judgment. Relying solely on one test is insufficient and can lead to misdiagnosis. If you suspect you might have Lyme disease, consult a healthcare professional for appropriate evaluation and testing, taking into account your symptoms, exposure history, and other relevant factors. Tags: CDC CSF ELISA IFA Immunofluorescence Assay Lyme Disease PCR Testing | |||
| |||
| | |||
|
 3350
3350