| Allergies and asthma are common childhood conditions often linked, with allergies frequently being a trigger for asthma attacks. Allergic reactions, caused by an overreaction of the immune system to harmless substances like pollen, dust mites, or pet dander, can inflame the airways, leading to asthma symptoms such as wheezing, coughing, shortness of breath, and chest tightness. Children with allergies are at a significantly increased risk of developing asthma, and managing allergies effectively is crucial in preventing and controlling asthma symptoms. Treatment typically involves allergen avoidance, medications like antihistamines and inhaled corticosteroids, and in some cases, immunotherapy. 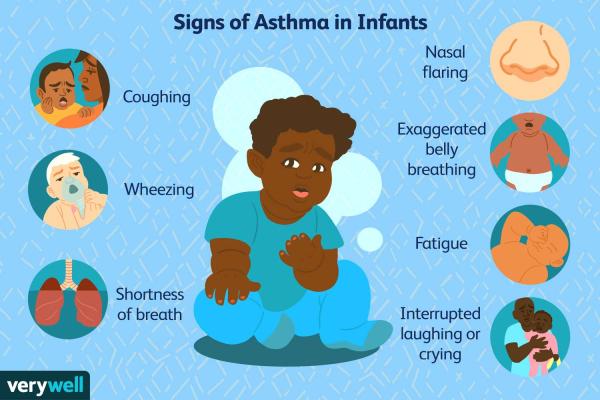
Allergies and asthma are common childhood conditions that often coexist. They're both inflammatory diseases, meaning they involve swelling and irritation of the airways and other tissues. While distinct, they share many overlapping triggers and symptoms, sometimes making diagnosis and management complex.
Allergies in Children: - What are they? Allergies occur when the immune system overreacts to a harmless substance (allergen) like pollen, dust mites, pet dander, food, or insect venom. This overreaction causes the release of histamine and other chemicals, leading to symptoms.
- Common symptoms: Runny nose, sneezing, itchy eyes, rash (hives), eczema (a skin condition), swelling, and in severe cases, anaphylaxis (a life-threatening reaction). Food allergies can cause vomiting, diarrhea, and abdominal pain.
- Diagnosis: A pediatrician will often use a detailed medical history, physical exam, and allergy testing (skin prick tests or blood tests) to identify allergens.
- Management: Avoidance of allergens is key. This may involve changes to the home environment (e.g., dust mite covers, air purifiers), dietary restrictions (for food allergies), and medication like antihistamines or nasal corticosteroids. In severe cases, immunotherapy (allergy shots) may be considered.
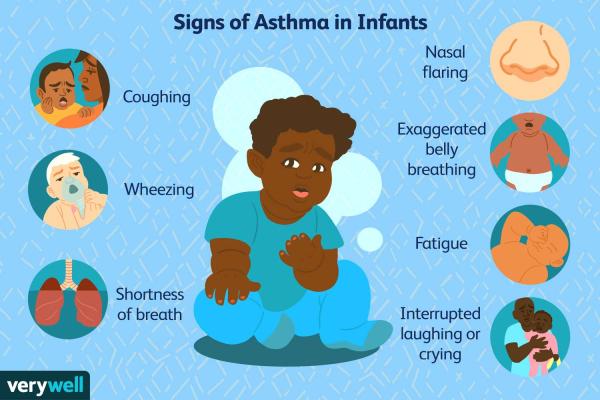
Asthma in Children: - What is it? Asthma is a chronic lung disease characterized by inflammation and narrowing of the airways. This makes breathing difficult, causing wheezing, coughing, shortness of breath, and chest tightness.
- Common triggers: Allergens (often the same as those causing allergies), respiratory infections, exercise, cold air, irritants (smoke, pollution), and stress.
- Diagnosis: Diagnosis involves a physical exam, reviewing symptoms, and lung function tests (spirometry).
- Management: Involves using inhalers (bronchodilators to open airways and corticosteroids to reduce inflammation), avoiding triggers, and developing an asthma action plan to manage exacerbations. Regular check-ups with a pediatrician or pulmonologist are crucial.
The Link Between Allergies and Asthma:
Children with allergies are at a significantly higher risk of developing asthma. The inflammation triggered by allergic reactions can make the airways more sensitive and prone to asthma attacks. This is often referred to as the "allergic march," where allergies often precede the development of asthma.
Important Considerations: - Early diagnosis and management: Early intervention is vital for both allergies and asthma to prevent complications and improve quality of life.
- Individualized treatment plans: Treatment plans are tailored to the individual child's specific allergies and asthma severity.
- Parental education: Parents play a crucial role in managing their child's allergies and asthma, understanding triggers, recognizing symptoms, and administering medications correctly.
- Emergency preparedness: Children with severe allergies or asthma should have a plan in place for managing emergencies, including access to epinephrine (for anaphylaxis) and understanding when to seek immediate medical attention.
This information is for general knowledge and does not constitute medical advice. Always consult with a pediatrician or allergist for diagnosis and treatment of allergies and asthma in children.
Tags: Allergic Asthma Allergies Asthma  
|
 1,352
1,352  0
0  0
0  3350
3350